Varicose Vein Solutions
Sydney Vascular Surgeon - Dr Mayo Theivendran
What are the benefits of varicose vein surgery?
Varicose vein surgery offers a range of benefits:
- Improved aesthetics: Surgery can help restore the appearance of your legs by removing or minimising unsightly varicose veins.
- Pain relief: Surgery can alleviate the pain, aching and discomfort associated with varicose veins.
- Prevention of complications such as leg ulcers and blood clots.
- Enhanced blood flow: Surgery helps improve blood flow in the affected areas, promoting overall leg health.
- Increased mobility: With reduced discomfort and improved blood circulation, you may experience better mobility and quality of life.
Types of varicose veins surgery
Dr Theivendran employs several procedures to treat varicose veins. The choice of procedure depends the severity of the condition, the affected vein/s, your overall health and your personal preference. Here are the solutions Dr Theivendran recommends:
1. Cutera Laser Therapy
Cutera® laser treatment is a minimally invasive procedure that uses advanced laser technology to treat varicose veins and spider veins.
The laser delivers focused energy to close off the veins without the need for incisions. It’s a relatively quick and generally well-tolerated procedure with minimal discomfort.
How Cutera® laser therapy is performed
The laser delivers pulses of light energy which cause the blood inside the veins to coagulate, eventually destroying the veins which are later reabsorbed by the body.
It feels like a quick rubber band snapping against your skin. A cooled treatment tip protects and provides additional comfort.
You’ll usually see results after 1 to 3 sessions.

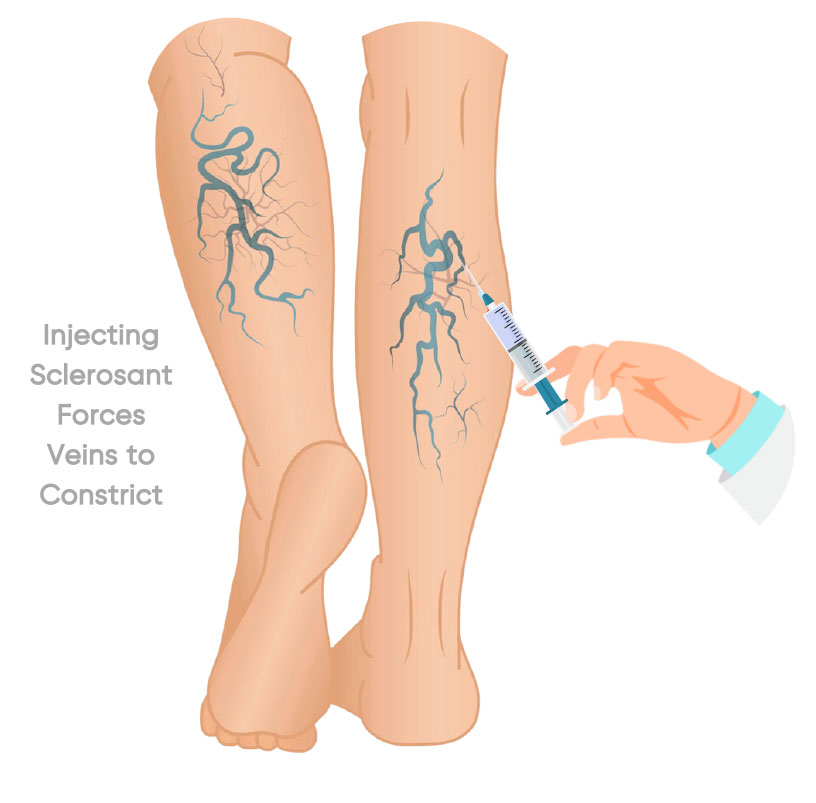
2. Sclerotherapy
Sclerotherapy is another minimally invasive procedure used to treat both varicose veins and tiny spider veins.
How sclerotherapy is performed:
- After numbing the area with local anaesthetic, Dr Theivendran injects a special solution directly into the affected veins using a very fine needle. This solution irritates the veins’ inner linings, causing them to seal shut.
- Over time, the closed veins are gradually absorbed by the body, and blood flow is rerouted through healthier veins.
Sclerotherapy is an outpatient procedure, and you may need multiple sessions. You can resume normal activities shortly after each session.
Learn more about Sclerotherapy treatment available at Harbour Vascular
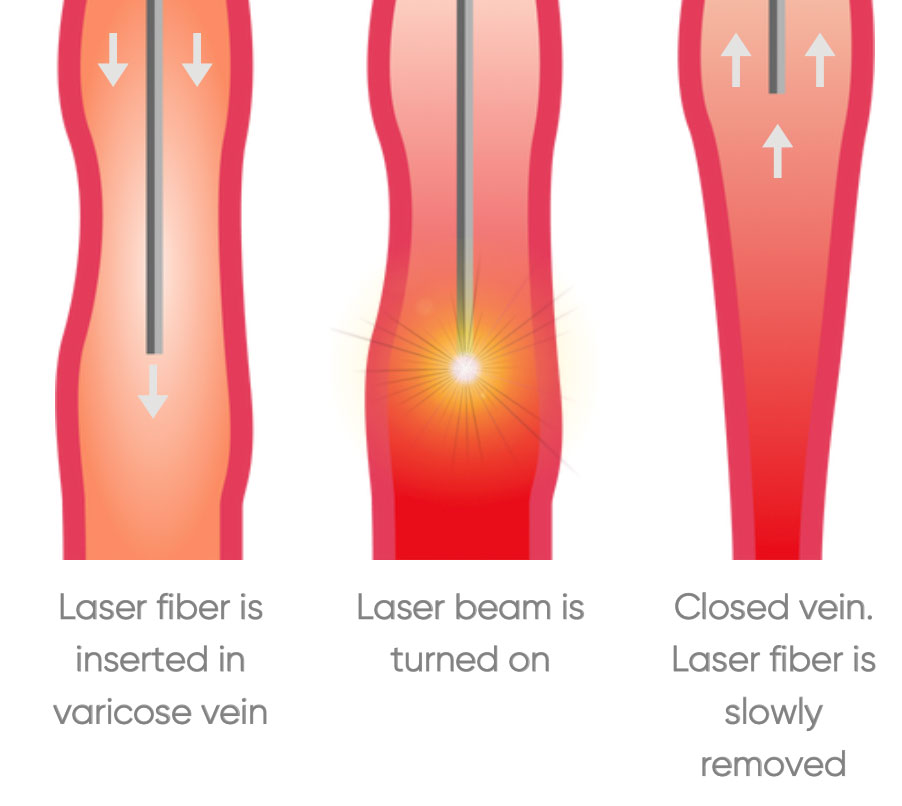
3. Endovenous laser treatment (EVLT)
EVLT is a minimally invasive procedure used to treat varicose veins. This method is popular due to its effectiveness and relatively swift recovery times. How EVLT is performed:
- Dr Theivendran injects local anaesthetic to numb the treatment area. Alternatively, general anaesthetic may be used.
- Using ultrasound guidance, he makes a small incision near the vein and positions a laser fibre in the incision.
- Once the laser fibre is correctly placed, laser energy is emitted into the varicose vein. This heats and seals the vein, causing it to close.
- After the procedure, the incision is closed, usually with a small bandage or a few stitches. You can usually return home shortly after the surgery.
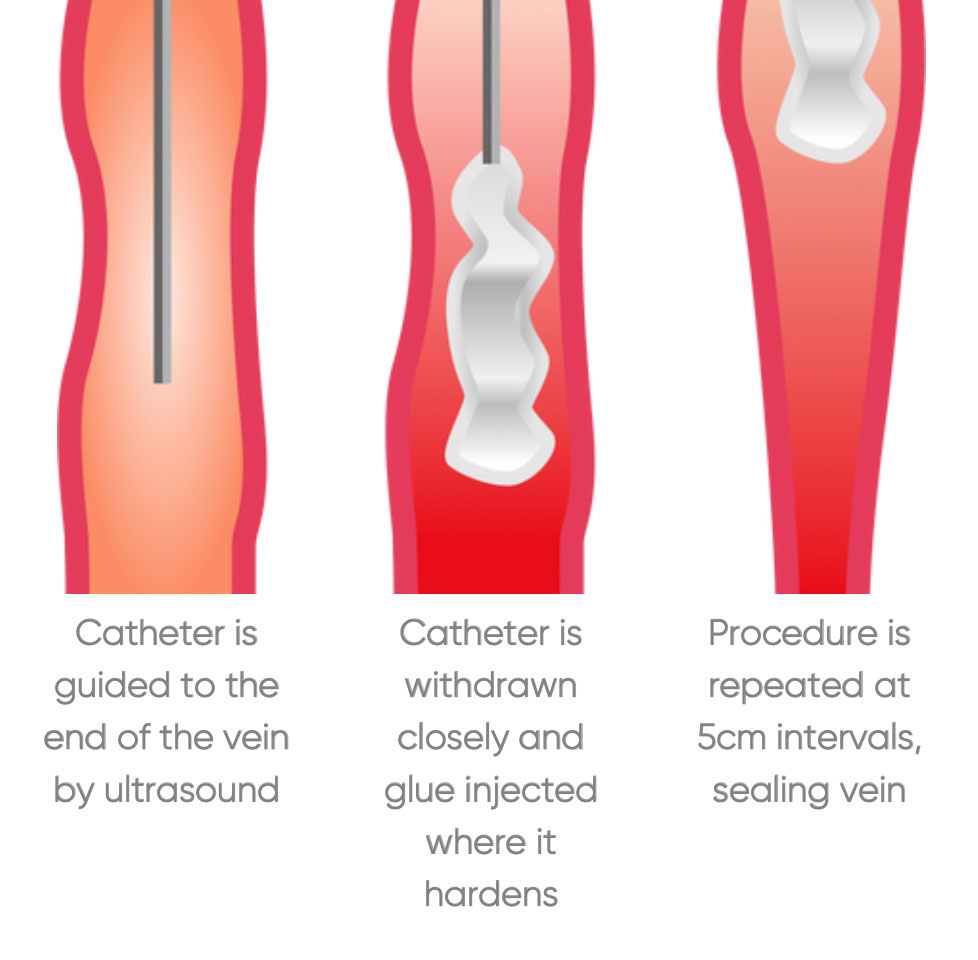
4. Endovenous glue treatment
This is a relatively new, minimally-invasive procedure involving the application of a medical-grade adhesive, such as VenaSeal®, directly into the affected vein using a catheter. The adhesive seals the vein shut, effectively closing it off.
How endovenous glue treatment is performed:
- First, Dr Theivendran numbs the area using local anaesthetic. Alternatively, general anaesthetic may be used.
- He makes a tiny incision near the varicose vein's entry point, usually in the lower leg. A catheter is then inserted into the affected vein under ultrasound guidance.
- A medical-grade adhesive is injected into the vein through the catheter. The adhesive functions to seal the vein from the inside.
- The glue quickly solidifies upon contact with blood, causing the vein to close and prevent further blood flow.
- After the glue is deposited, Dr Theivendran carefully removes the catheter and covers the entry point with a small bandage.
You can usually return to your regular activities within a short period.
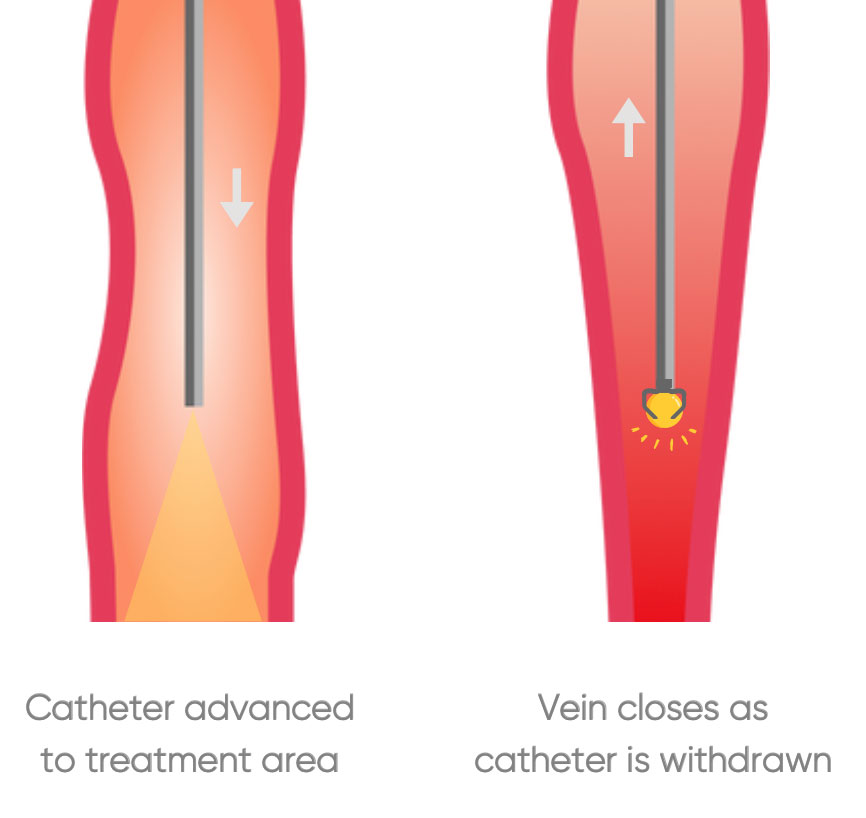
5. Radiofrequency ablation (RFA)
RFA is another minimally invasive technique for treating varicose veins. It employs radiofrequency energy to heat and close the affected vein.
How RFA is performed:
- Similar to EVLT, RFA typically requires local anaesthesia or general anaesthetic.
- Using ultrasound guidance, Dr Theivendran places a catheter (thin tube) into the varicose vein and injects a solution to separate the skin and nerves from the vein.
- The catheter contains a device that emits radiofrequency energy. This energy heats and seals the vein, causing it to collapse.
- After the procedure, he removes the catheter. The incision site is closed with a small bandage or a few stitches. You can usually go home shortly after the procedure.
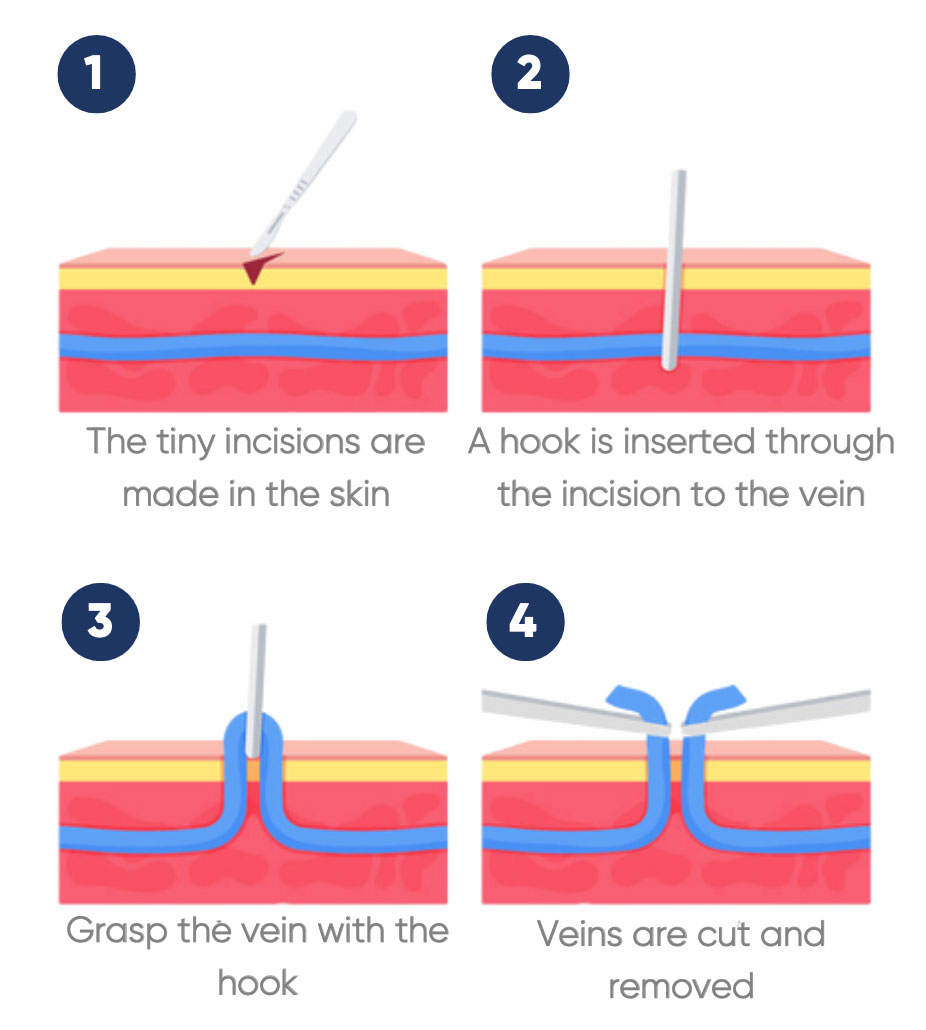
6. Ambulatory phlebectomy
Ambulatory phlebectomy is specifically designed for the removal of smaller varicose veins. It's typically performed on an outpatient basis with minimal down-time.
How ambulatory phlebotomy is performed:
- General anaesthesia is administered so you’re unconscious.
- Dr Theivendran makes several tiny incisions along the path of the varicose vein. These incisions are usually quite small, often just a couple of millimetres long.
- Special tools are used to grasp and remove the varicose vein through the tiny incisions.
- After the vein has been removed, the small incisions are usually left to heal without the need for sutures.
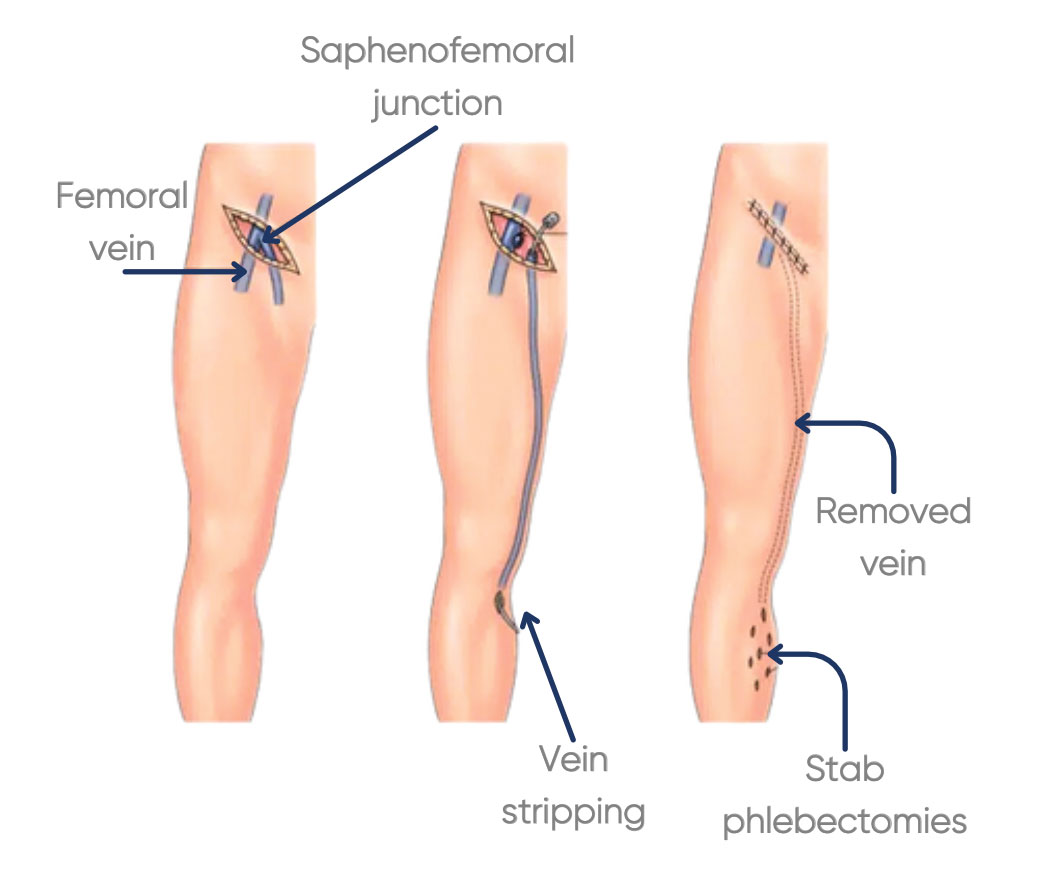
7. Surgical ligation and stripping
Surgical ligation and stripping is a more traditional surgical method used for varicose vein removal. While less commonly employed today, it remains an effective option.
How surgical ligation and stripping is performed:
- General anaesthesia is administered so you’re unconscious.
- Dr Theivendran identifies the varicose vein and marks the areas for incisions.
- He ties off the varicose vein at two points – one near the groin and the other near the calf. This prevents blood from flowing through the vein.
- He then makes small incisions over the marked areas and uses a special tool to remove the problematic vein. The vein is pulled out through the incisions.
- After the vein has been removed, he closes the incisions with sutures, and applies dressings.
8. High ligation and vein bypass
Dr Theivendran performs high ligation and vein bypass when the great saphenous vein is causing significant issues. This is the main vein that runs from your foot up to your thigh.
How high ligation and vein bypass is performed:
- High ligation and vein bypass procedures are generally performed under general anaesthesia so you’re unconscious.
- Dr Theivendran ties off the great saphenous vein near the groin to stop blood flowing through it.
- He then creates a bypass, typically using a synthetic graft or a healthy vein from your own body. This graft is attached to the blocked portion of your great saphenous vein, redirecting blood flow.
Varicose vein surgery aftercare
Aftercare following varicose vein surgery varies depending on the type of surgery you’ve had and your personal health. Dr Theivendran’s instructions may include:
- Leg elevation: For the initial few days, elevate your legs whenever possible, keeping them above heart level to minimise swelling and promote proper venous circulation.
- Compression stockings: Dr Theivendran may recommend wearing compression stockings to reduce swelling and improve blood flow. Follow his guidance on when and how to wear them.
- Medications: Take prescribed pain relievers and antibiotics as directed to manage discomfort and prevent infection.
- Wound care: Keep the incision sites clean and dry. Follow Dr Theivendran's instructions regarding dressing changes and bathing. Watch for any signs of infection, such as increased redness, warmth, pus at the incision sites or fever.
- Mobilise: Engage in light, regular activities as advised by Dr Theivendran. Gradually resume your daily routine but avoid strenuous exercise such as running or swimming.
- Follow-up appointments: Attend all scheduled follow-up appointments. These visits are essential for monitoring your progress and addressing any concerns.
- Adopt healthy habits. Maintain a balanced diet, stay hydrated, and monitor your weight. Regular exercise, such as walking, can help improve your vascular health.
What to expect after varicose vein surgery

Bruising and swelling. It's common to experience some bruising and swelling at the surgical site, which should subside over time.

Numbness over the treated vein which will resolve over 6-12 months.

Scarring may develop at the incision sites after open surgery, although it is usually minimal.

Recurrence: About 20% of people who’ve had varicose veins in the past will develop others in the future.
Complications of varicose vein surgery
While varicose vein surgeries are generally safe and effective, complications can occur. They include:

Infection: This is a rare complication but is more likely if you had skin ulcers.

Nerve injury: In rare cases, nerve injury or damage can occur, leading to numbness or tingling.

Blood clots while rare, can form in the deep veins of the legs, leading to deep vein thrombosis (DVT).

Allergic reactions: Some people experience allergic reactions to anaesthesia or medications used during surgery.
Success rates of varicose vein surgery
Success rates vary depending on the individual procedure:
- Endovenous: 98% success
- Open Surgery: 98% success
- Sclerotherapy alone: 65% (may require multiple sessions)
How Dr Theivendran can help
If varicose veins are affecting your quality of life, ask your treating doctor for a referral to Dr Theivendran, an experienced Vascular and Endovascular Surgeon.
He will assess your condition and, if appropriate, discuss surgical options that can bring you lasting relief and peace of mind.
If you have any questions, please don't hesitate to contact our rooms on (02) 9066 6547
For appointments and enquiries:
Monday - Friday: 8:00am to 4:30pm
Fax: (02) 9182 7533